The Convergence of mHealth and Accountable Care
It’s easy to see that G. Daniel Martich, M.D., chief medical information officer at the University of Pittsburgh Medical Center (UPMC), like many of his cohorts at the large integrated healthcare system and elsewhere in the industry, can see the big picture.
Dr. Martich, who is also a member of the Healthcare Informatics editorial advisory board, is focused squarely on accountable care, and better yet, he has an idea on how to get there. At HIMSS13, on the same day that was officially themed after “patient engagement,” Martich spoke with HCI Associate Editor Gabriel Perna on why this year at the annual conference he has really zeroed in on patient engagement and mobile health (mHealth).
“How we engage the patient in their own care ties into accountable care because we can’t continue to deliver the same care at hospitals, critical care units, and in emergency departments as we used to, because we can’t afford to,” Martich says. “So how do we care for those patients in a better, if not equal setting, moving them first to the outpatient center then the home? We need patients to engage. How do they do that? They can engage with a laptop or a desktop, but the reality is patients are engaging more and more with mHealth.”
At UPMC, Martich says the organization is attempting to extend this concept in a mobile fashion to their patient base in the ambulatory setting. The organization, he says, is working on a marketing effort that attempts to get patients to sign up for their shared personal health record. This means the patient sees what the doctor sees in terms of medications, upcoming appointments, and prescriptions.
Already, Martich says, the organization has gotten 150,000 patients on board. Furthermore, UPMC will be extending this mobile app to those who use the organization’s insurance product. Half of those patients don’t have a UPMC physician. But that doesn’t matter, as the organization is essentially an accountable care organization (ACO), he notes.
G. Daniel Martich, M.D.
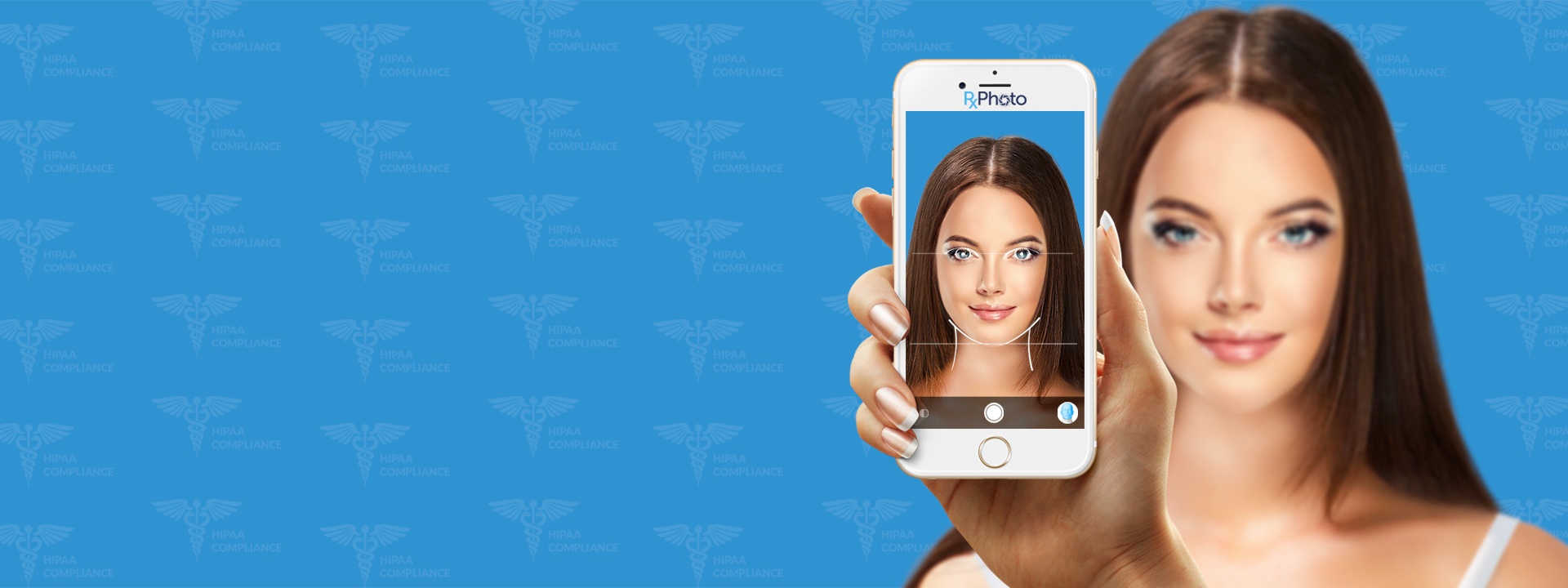
“We have an insurance arm, we have a hospital division, and we have a physician division. Tying all of those together and going out beyond that is obviously a big step. And [it’s about] developing the tools and strategies around that, so you can do virtual care collaboration using the camera on a laptop and the camera on an iPhone. If you want to see the [practitioner], you can see the [practitioner],” Martich says.
ACOs, Martich says, are about access, quality care, and reasonable cost. Both UPMC and the UPMC Health Plan in this regard are incentivized to reduce costs, and one of the best ways to do that is to keep the patient out of the hospital. The mHealth is one way to do that, as is UPMC’s electronic visits (eVisits), a growing online platform at which has actually integrated with the mobile app. There are also non-technology answers, he says, such as extended hours clinics, which can keep a patient out of the emergency department.
“We still want to admit people to the ER, if they need to go. But we don’t want a system where people say, ‘My doctor is not available, so I’m defaulting to the most convenient option.’ That option happens to be the most expensive option. In reality, the most convenient option should be the least expensive option,” Martich says.